Pancreatic Cancer: A disease with few therapeutic options
According to Globocan 2022 estimates, pancreatic cancer represents 2.56% of all cancer cases. This disease usually causes no symptom early on, often resulting in death within a relatively short period of time. The causes and risk factors for this cancer are multiple. Since the chances of survival are low, treatments are generally aimed at slowing the development of the tumour. Progress are expected in the early detection of this cancer, in the development of new treatments or new therapeutic approaches. The blood-based diagnostics developed by Acobiom enable to predict the patient response to the main first-line therapies available for pancreatic cancer..

About the Pancreas
The pancreas is a gland located deep in the abdomen, between the stomach and the spine.
It is made up of exocrine cells and endocrine cells, and it is often described as having a head, body and tail..
The pancreas produces enzymes that aid in digestion (thanks to exocrine cells) and makes insulin and other important hormones (thanks to endocrine cells) that help the body absorb sugar and control blood sugar.
What Is Pancreatic Cancer?
Pancreatic
cancer develops when cells of the organs grow out of control, developing a
tumor.
About 95 % of pancreatic cancers are exocrine tumors, beginning in the exocrine cells of the organ. 80% of these exocrine tumors starts in the exocrine cells that line the ducts of the pancreas. Hence, these types of cancer are called pancreatic ductal adenocarcinomas.
About 5% of pancreatic tumors are neuroendocrine tumors (NET), also called islet cell tumors. There are many subtypes of this type of tumor. They often grow slower than exocrine tumors, and are most often benign.
There is no specific cause for this cancer, but there are risk factors that can increase the likelihood of disease development.
Pancreatic cancer is usually detected late.
The diagnosis of this cancer is made after a combination of clinical examinations, imaging tests, blood tests and tumor tissue. These tests and analyses also make it possible to establish the stage of the disease’s progress.
There is not yet a biological marker that can reliably diagnose pancreatic cancer.
The treatment of these tumours is based on their growth stage.
Standard treatments are surgery, chemotherapy, radiotherapy or a combination of these treatments.
The chances of survival or healing are low.
Only surgery (possible for about 20% of patients), combined with chemotherapy, can lead to the remission of this cancer.
How many people have pancreatic cancer?
According to the International Agency for Research on Cancer (World Health Organization), pancreatic cancer accounts for 2.56% of all cancer cases worldwide.
It is the 12th most common cancer, and the 6th leading cause of cancer deaths worldwide.
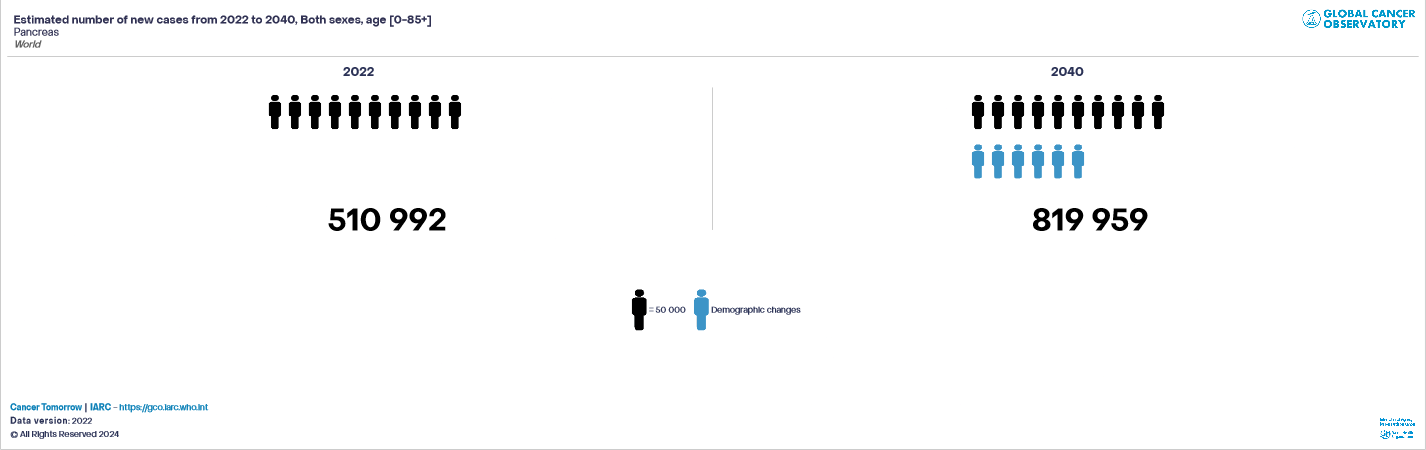
In 2022, pancreatic cancer accounted for 510,992 cases worldwide, resulting in 467,409 deaths.
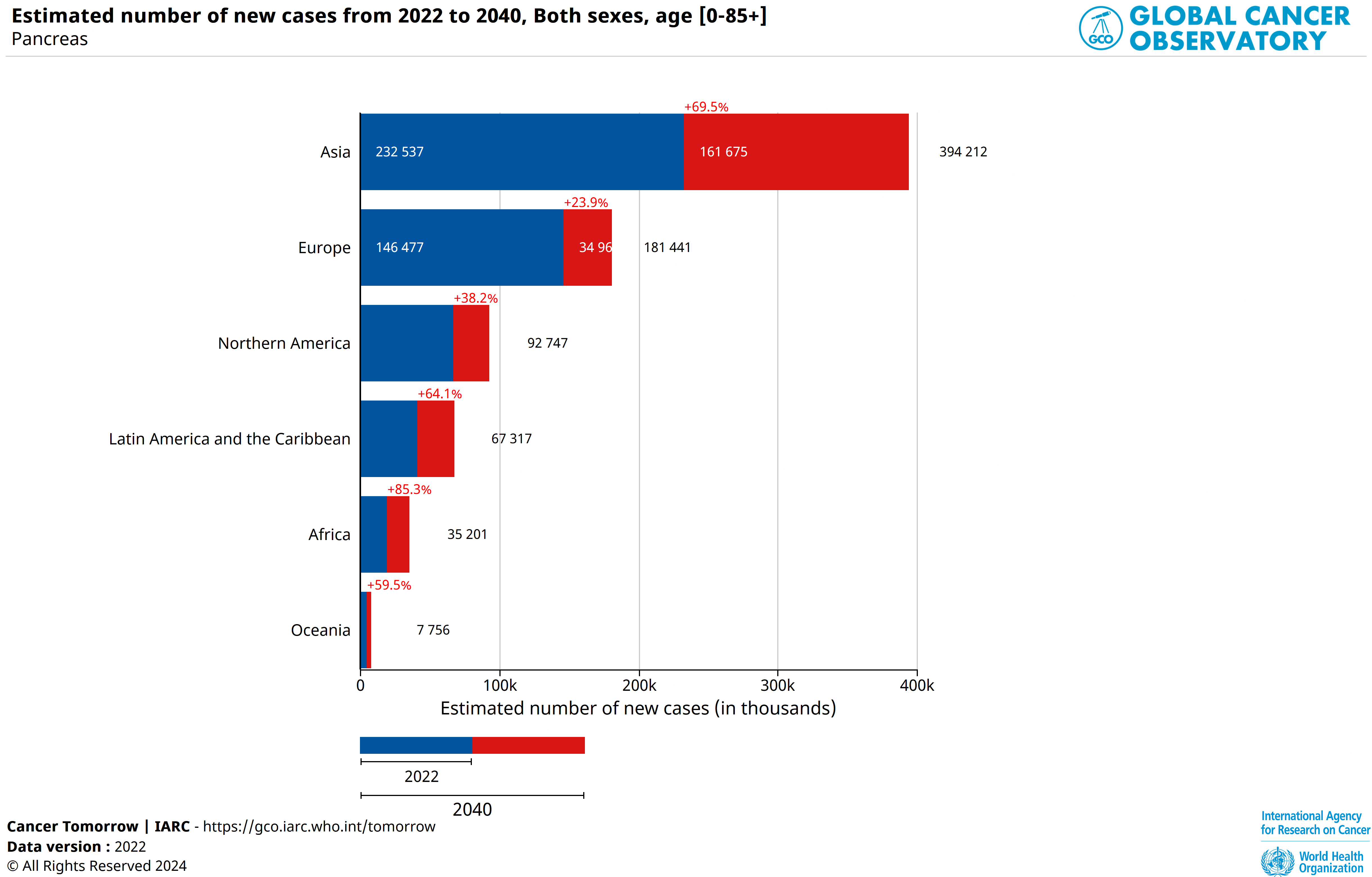
In 2022, 146,477 cases were reported in Europe, 67,089 cases in North America, and 232,537 cases in Asia (118,672 cases in China, 47,627 cases in Japan).
It is also important to note that pancreatic cancer is more frequent with age (68% of pancreatic cancer cases appear after age 65), and slightly more frequent in men (53% of cases) than in women (47% of cases).
Is the number of pancreatic cancer cases increasing?
The incidence of Pancreatic Cancer has markedly increased over the past decades.
According to IARC (Globocan), this cancer is one of the few that is constantly increasing in the world: 510,992 cases were recorded in 2022, the number is expected to reach 819,959 cases in 2040.
According to certain sources (PANCAN, etc.), pancreatic cancer could become the second leading cause of cancer mortality in the European Union and the USA. Deaths from this disease are thus set to continue rising worldwide.
What is the life expectancy with pancreatic cancer?
Patients diagnosed with pancreatic cancer generally have an unfavourable prognosis.
The chances of survival are low in part because this cancer usually causes no symptoms in its early stages, resulting in metastatic disease at the time of diagnosis.
Median survival (or lifespan) after diagnosis is less than one year; 5-year survival is about 5-10% and complete remission is still extremely rare (American Cancer Society, 2008).
What is the situation of pancreatic cancer in comparison to other cancers?
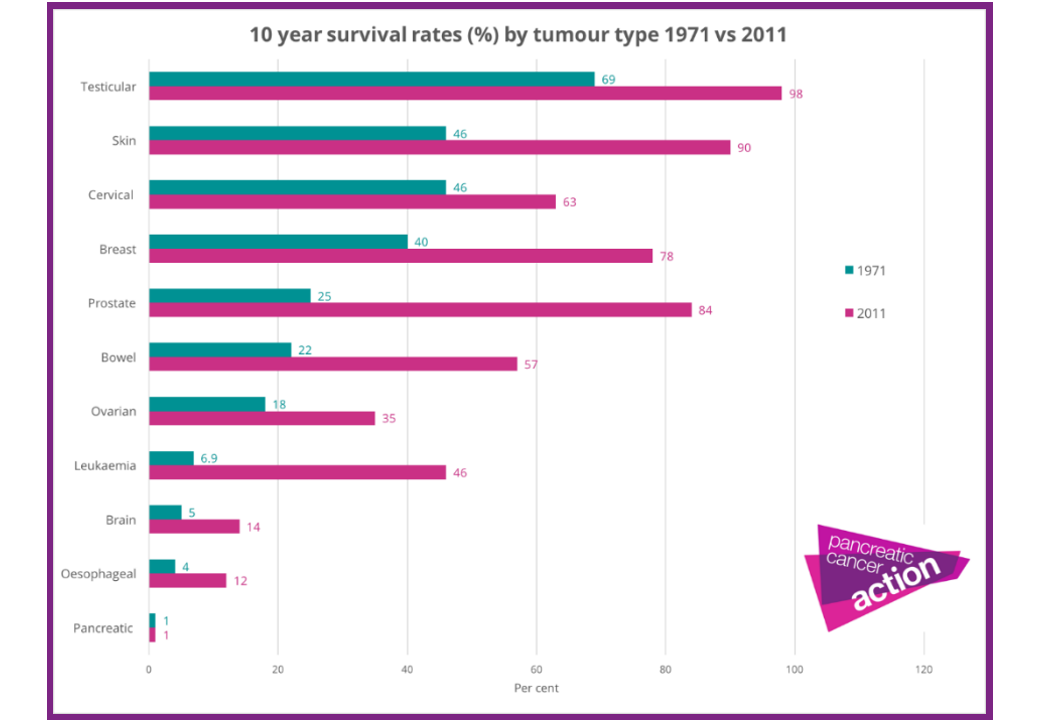
The impact report of the British charity Pancreatic Cancer Action (2015) highlights the lack of progress in the fight against pancreatic cancer for several years. Hence, the 10-year survival rate remains at similar levels to those seen in the 1970s.
To compare with breast cancer (same stages III and IV), the 5-year survival rate for women is close to 72%.
By contrast, while overall cancer mortality decreased in the UK during the past 10 years, mortality due to pancreatic cancer increased by 8%. Across the Europen Union, pancreatic cancer survival in 2017 is similar to that of the United Kingdom.
What are the causes of pancreatic cancer?
Cancers, and pancreatic cancer in particular, are complex biological phenomena and are generally due to a combination of causes.
Cancers can be the result of one or more risk factors, even though these diseases can developed in people with no risk factors.
The incidence and prevalence of pancreatic cancer vary widely within and between countries. These disparities result from genetic differences, as well as exposure to certain environmental risk factors.
For instance, levels of smoking, alcohol consumption, as well as the number of people with diabetes and obesity are different in Europe, which contributes to the variation in the incidence of pancreatic cancer.
What are the risk factors for pancreatic cancer?
A risk factor is a parameter that can increase the probability of a pathology or trauma occurring. On the other hand, the presence of a risk factor does not necessarily imply the occurrence of the pathology with which it is associated.
In the case of pancreatic cancer, different risk factors have been identified with varying degrees of certainty. These can be classified into two categories: factors inherent to the individual and environmental factors.
One of the risk factors inherent in the individual is age. Indeed, there is a peak in the onset of pancreatic cancer between the ages of 65 and 85, with a low probability of the disease occurring before the age of 50.
Some risk is also related to family predispositions or genetics. Examples of genetic mutations include the BRCA2 and CDKN2A genes.
Finally, blood groups A, AB and B may also have a higher risk of developing pancreatic cancer.
One of the environmental risk factors is tobacco: a threefold increase in the risk of developing pancreatic cancer, with the risk increasing with consumption and duration of smoking.
The scientific community established a list of risk factors that may increase the chances of developing a pancreatic cancer. But, as mentioned by Pancreatic Cancer UK, “it’s important to remember that having some of the risk factors doesn’t mean you will definitely get pancreatic cancer”.
The risk factors for pancreatic cancer are:
> Age (chances increase with age, most being 60+),
> Smoking,
> Obesity,
> Family history of pancreatic cancer,
> Chronic pancreatitis and hereditary pancreatitis,
> Diabetes (risk increased with long-term, 5+ years),
> Chronic, heavy alcohol use
> Diet (high in red and processed meats),
> Gender (More men are diagnosed with pancreatic cancer than women),
> Blood group (blood groups A, AB and B may have a higher risk),
> Race and ethnicity (Black people or Ashkenazi Jewish are more likely to develop pancreatic cancer).
However, pancreatic cancer can develop in a person who does not have any of the risk factors listed.
What are the main signs and symptoms of pancreatic cancer?
Pancreatic cancer does not cause generally any signs or symptoms in the early stages of the disease.
As cancer develops, it can cause signs, symptoms, or indications related to the pancreas or other organs of the digestive system.
Symptoms of this cancer vary according to its location in the pancreas: head, body or tail, and the location of the functions the tumor cells: exocrine cells or endocrine cells.
The following symptoms may indicate the development of a pancreatic cancer:
> Pain, usually in the abdomen or back,
> Unexplained weight loss,
> Jaundice,
> Recent-onset diabetes,
> Loss of appetite,
> Indigestion,
> Nausea,
> Changes in stool,
> Pancreatitis,
> Blood clots
> Abdominal bloating or Stomach bloating.
> Fatigue, weakness and depression are also symptoms.
But all these symptoms are always associated with the development of a pancreatic cancer.
How to detect pancreatic cancer?
There is no standard test to detect pancreatic cancer, which makes it difficult to diagnose.
In the current practice, pancreatic cancer is usually diagnosed by a combination of clinical examinations, imaging tests (computed tomography (CT) scan, magnetic resonance imaging (MRI), Positron Emission Tomography (PET) Scan, Endoscopic Retrograde Cholangiopancreatography (ERCP), endoscopic ultrasound (EUS), Laparoscopy), a blood test measuring a biological marker, carbohydrate antigen 19-9 (CA19-9, not specific) and an invasive biopsy to obtain a sample of the tumor tissue to establish the correct diagnosis.
What are the Pancreatic Cancer markers?
Depending on the signs and symptoms caused by a suspicion of pancreatic cancer, several exams and tests will be performed establish the diagnosis.
If the cancer is confirmed, more tests will be done to help determine the stage (extent) of the cancer.
There is no blood test or specific tumour markers to diagnose a pancreatic tumour. For example, a blood test measuring carbohydrate antigen 19-9 (CA19-9) is usually performed, but this biological marker is not specific to pancreatic cancer..
A pancreatic exocrine tumor can cause higher bilirubin and liver enzyme levels in the blood. High levels of these substances in blood can suggest a pancreatic cancer, but these markers do not happen in all pancreatic cancer patients.
A pancreatic neuroendocrine tumors (PNETs) can be detected in measuring the following markers:
> Chromogranin A (cgA, high in most people with PNETs),
> Pancreatic polypeptide (PP, often high in people with PNETs),
> Other specific hormones made by pancreatic neuroendocrine tumors.
What are the stages of a Pancreatic Cancer?
The stage
of a cancer describes how the disease has been developing, how it is serious
and how best to treat it.
The
earliest stage pancreas cancers are stage 0 (carcinoma in situ), and then range
from stages I (1) through IV (4). In general, the lower the number, the less
the cancer has spread or is difficult to treat.
In Pancreatic
Cancer, the stage of the disease is based on 3 data:
1 – The extent of the tumor (T)
2 – The spread to nearby lymph nodes (N) 3 – The spread (metastasized) to distant
sites (M)
Other
factors are measured to determine the prognosis of the disease:
a) the tumor grade (from 1 to 3),
b) the extent of resection (from R0 to
R2).
What are the main therapies to treat Pancreatic Cancer?
Standard treatments are surgery, chemotherapy, radiation, or a mix of these.
As pancreatic cancer is generally detected when tumor cells are spread over the pancreas or when the tumor is began metastatic, the decision-making model is a balance between the patient’s medical condition (side effects, patient’s preferences, and overall health) and the intrinsic characteristics of the cancer (type, spread and stage of the tumor).
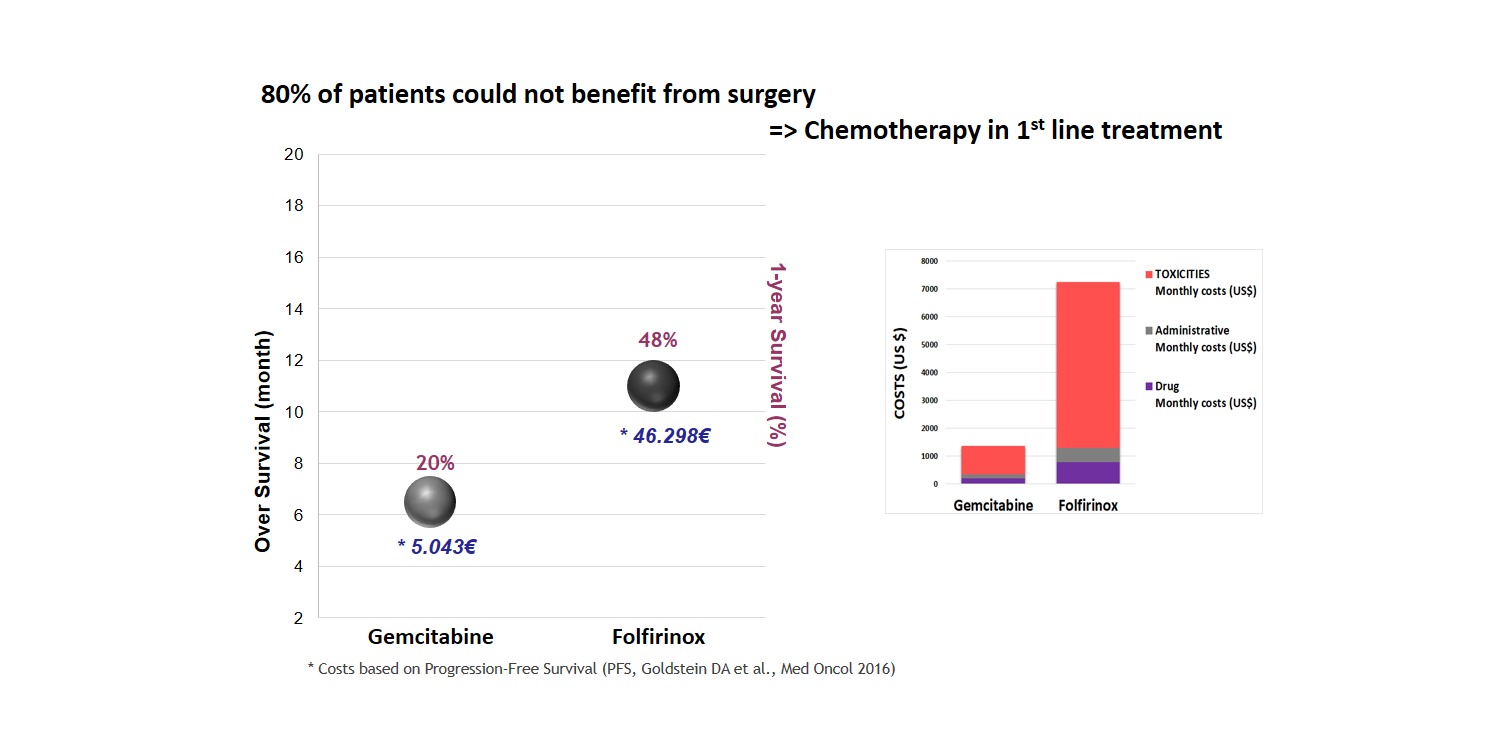
The surgery option is chosen to remove the tumor or when a part of the tumor can be resected with the objective to relieve symptoms. About 20% of patients with pancreatic cancer can benefit from a surgery. Surgery is the only potentially curative treatment option in pancreatic cancer treatment.
In pancreatic cancer treatment, chemotherapy is used to kill cancer cells or reduce the tumor size before surgery or radiation therapy.
Several chemotherapy drugs are used for pancreatic cancer: 5-fluorouracil (F-5U), Capecitabine, Gemcitabine, Nab-paclitaxel, Irinotecan, Oxaliplatin, etc., alone or in combination like: Gemcitabine + nab-paclitaxel, Gemcitabine+ Erlotinib, Folfirinox (5-flurouracil, leucovorin, irinotecan and oxaliplatin).
Here is a comparison of clinical results and the associated costs between Gemcitabine and Folfirinox treatments.
What kinds of progresses are forecasted to improve the therapy efficiency and the patient quality of life during treatment?
Ongoing clinical trials are investigating new types of treatments in the field of immunotherapy, RNA vaccines combined with chemotherapy, targeted therapy, precision medicine, etc.
As surgery offers today the best chance of controlling or treating pancreatic cancer, the early detection of this tumor is one of the major issues to improve treatment outcomes.
Another challenge is that pancreatic tumors are surrounded by a dense tissue layer, called the stroma. This makes it difficult for treatment to reach the tumor. Researchers are studying ways to get treatment through the stroma to make it more effective.
Also, some cancers have been successfully treated with targeted therapies which block specific mutations. But, these drugs have not been developed specifically for pancreatic cancer yet.
Molecular profiling can give information about the biology of the tumor. Results may align with targeted treatments that work well in other cancer types. As more studies are done, more targeted treatments will be developed and approved for pancreatic cancer patients whose tumors have specific molecular changes.
Molecular biomarkers (and diagnostic devices) are capable to predict patient response to a particular drug regimen. This approach could help choosing the most efficient therapy or the treatment with the less side effects, with the benefit to increase the patient overall survival and its quality of life during treatment.
To reach some of these objectives, Acobiom develops predictive blood-based diagnostics (Gemcitest®, Folfitest) for patient response to the main first-line therapies available.
Famous or anonymous, pancreatic cancer affects all people and all social categories.
Since pancreatic cancer has no direct cause, or direct link with the environment or lifestyle, the disease affects all people and social categories.
Many famous people have died of pancreatic cancer, including: Arno (singer), Syd Barrett, Johnny Clegg, Umberto Eco, Aretha Franklin, Dizzy Gillespie, John Hurt, Steve Jobs, Karl Lagerfeld, Michael Landon, Marcello Mastroianni, Claude Nougaro, Billy Paul, Luciano Pavarotti, Alan Rickman, Demis Roussos, Simone Signoret, Patrick Swayze …

